A year ago, she was tormented by advanced pancreatic cancer and advised by local doctors to “go home.” Today, she is living independently, full of energy and spirit. This extension of life represents the dedication and perseverance of countless healthcare professionals—and bears witness to the remarkable outcomes that can be achieved when advanced medical technology meets genuine human care.
From Helicobacter pylori to a “Mass”
Maureen (pseudonym), from Kenya, began experiencing abdominal discomfort in February last year. Local doctors initially suspected a Helicobacter pylori infection. However, after a period of anti-infective treatment, her pain did not improve. Sensing something was wrong, she underwent further examinations, and an ultrasound revealed a mass in the pancreas.
As a healthcare professional herself—and a breast cancer survivor—Maureen was acutely sensitive to the word “mass.” She immediately traveled to India for hospitalization. After a series of tests, she was confronted with a suffocating diagnosis: pancreatic adenocarcinoma, often referred to as the “king of cancers.”
Due to the tumor’s unfavorable location and large size, surgeons told her that open surgery was not an option. She was offered two alternatives: NanoKnife ablation or chemotherapy. At the time, Maureen had never even heard of NanoKnife. When she learned that the procedure could take up to eight hours, she firmly refused. “Limited experience, immature technique, long duration, and high risk”—that was her assessment then. Physically weak, she did not dare to undergo such a lengthy procedure and chose chemotherapy instead.
However, after four cycles of chemotherapy, the treatment showed minimal effect while the side effects were devastating. Seeking another evaluation from a gastrointestinal specialist, she was told, “This cancer may not be sensitive to chemotherapy.” She then underwent five sessions of stereotactic body radiotherapy (SBRT), but the tumor still failed to shrink. Her pain worsened, analgesics gradually lost effect, and her weight dropped from 70 kg to 54 kg.
“Doctors advised me to go home.”
Those words felt like a final verdict. Even Maureen, who had never wanted to give up, found herself on the brink of despair.
A Lifeline Across the Ocean
Hope emerged from the depths of desperation. Her nephew, who works in medical tourism, learned of her situation and quickly contacted the India office of Fuda Cancer Hospital, Guangzhou. After a comprehensive evaluation, the medical team proposed a new treatment strategy: a combination of NanoKnife ablation, interventional therapy, and immunotherapy.
After learning about Fuda’s extensive experience with NanoKnife technology, Maureen embarked on her journey to China in June this year. By then, her condition was extremely poor: no appetite, little will to live, and in her own words, “I didn’t even look like a human being anymore.”
Arriving late at night at the Fourth Medical Department of Fuda Cancer Hospital, the unfamiliar surroundings, jet lag, and relentless pain left her physically and emotionally exhausted. Yet a small, thoughtful gesture by the nursing staff—preparing a meal for her—instantly warmed her heart in a foreign land.
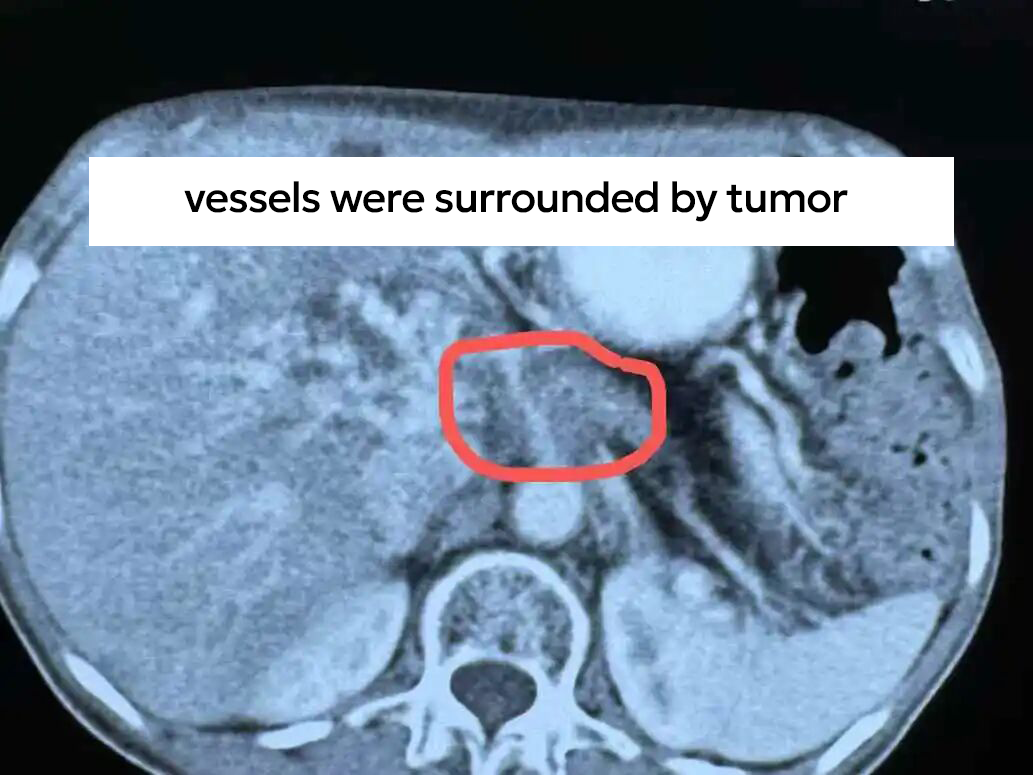
Examinations revealed that her pancreatic cancer was already at Stage III, with secondary malignant retroperitoneal lymph node involvement, making curative surgery impossible. Dr. Pang Xiaoming explained her condition clearly in plain language, patiently listening to her needs to tailor a more suitable treatment plan.

After multidisciplinary consultation, the team performed NanoKnife ablation of the pancreatic tumor combined with celiac plexus neurolysis. Postoperatively, immunotherapy was administered to control the tumor while alleviating cancer-related pain.


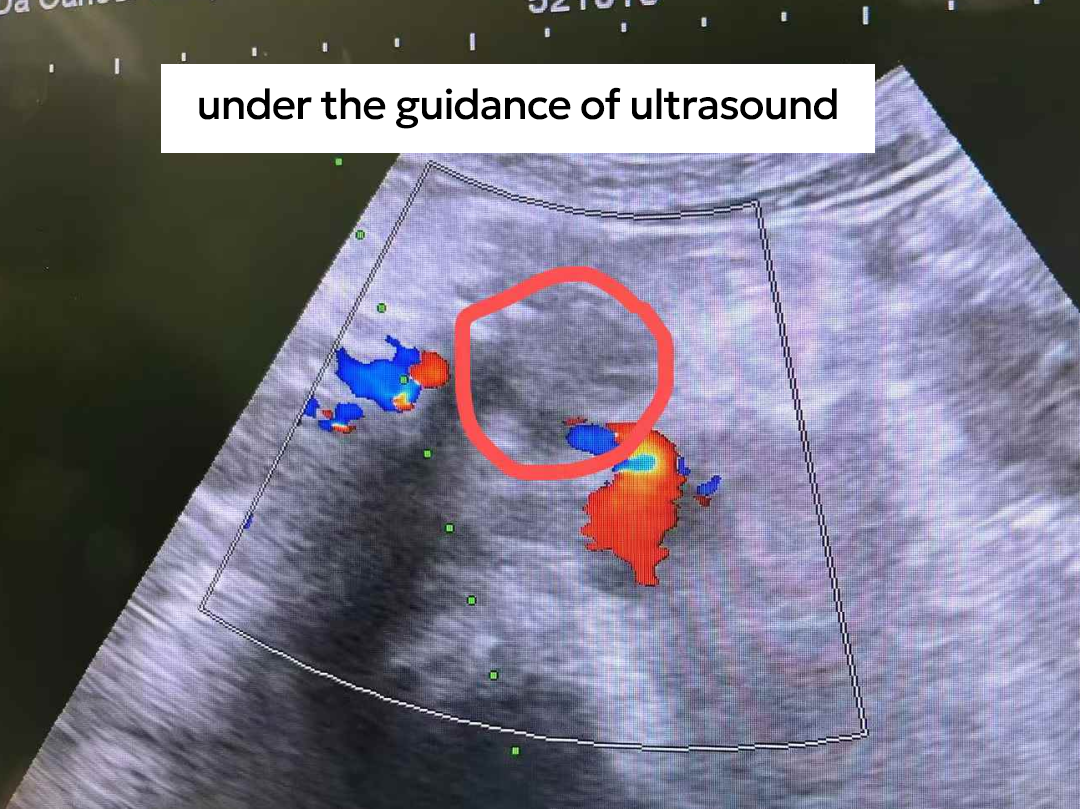
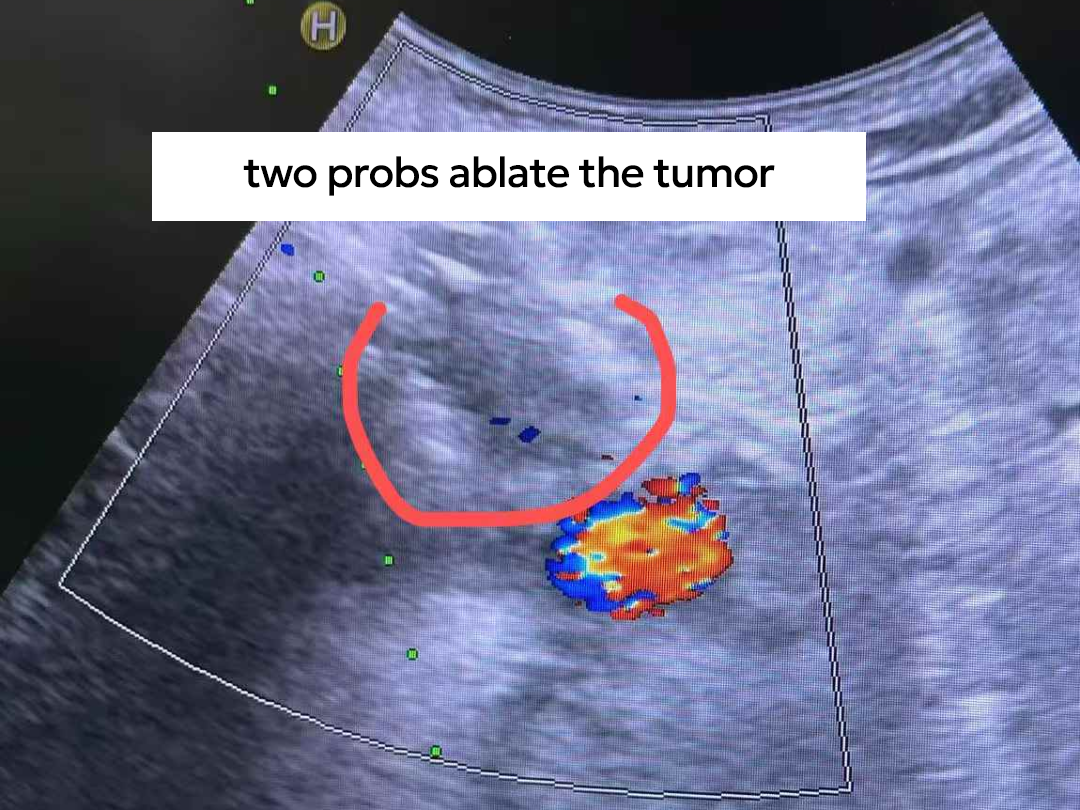
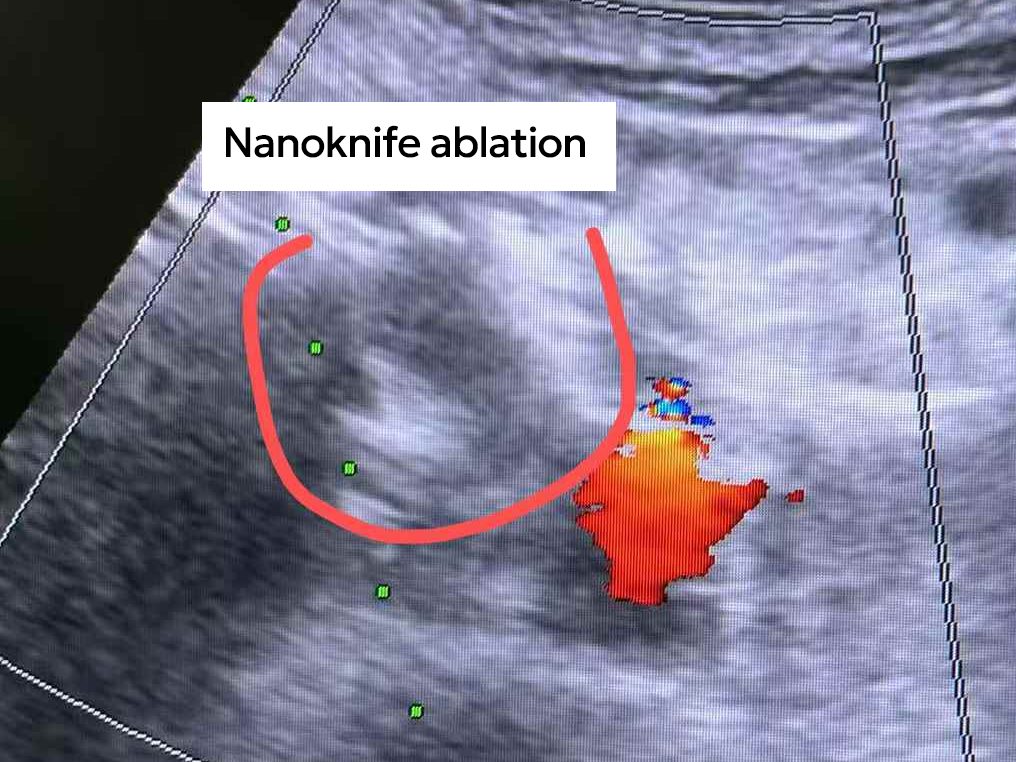
“NanoKnife ablation took less than an hour,” Maureen recalled—starkly different from the eight hours she had once feared. Even during her night of observation in the ICU, the warm companionship of the medical staff gave her a profound sense of security. In the days following surgery, miracles began to unfold: her appetite returned, she could sleep through the night, and her weight gradually increased. She later underwent arterial infusion chemotherapy.

“After returning home, I visited my original gastrointestinal doctor. He was shocked and said I must have received very high-quality treatment to have ‘come back to life,’” she said. Although the tumor had not shrunk dramatically and some marginal activity remained, most of the lesion was necrotic. More importantly, her strength, energy, and quality of life were all steadily improving. In the face of the “king of cancers,” Maureen had won a hard-fought battle.

A Dual Victory of Technology and Humanity
Maureen describes her journey with two “miracles”:
The first miracle was the exceptional medical expertise and humanistic care of the Fuda team—not only the efficiency of NanoKnife technology, but also the doctors’ and nurses’ willingness to listen and communicate with genuine empathy.
The second miracle was the comprehensive improvement of her body after treatment—a life-saving outcome created through the joint efforts of both doctors and patient.
Here, she felt true empathy from the medical staff, mutual support from fellow patients, and meticulous hospital services—from interpretation and transportation to thoughtful facilities such as a shared kitchen. All of this made her feel that she was “not trapped in a cage,” but instead empowered to fight cancer.

Her mindset transformed from resignation to openness. She hopes her experience can encourage other cancer patients:
“Don’t be afraid. There is always a method that suits you. Even in the darkest moments, never give up searching for the possibility of light.”

